Personalized Therapy of Cancer
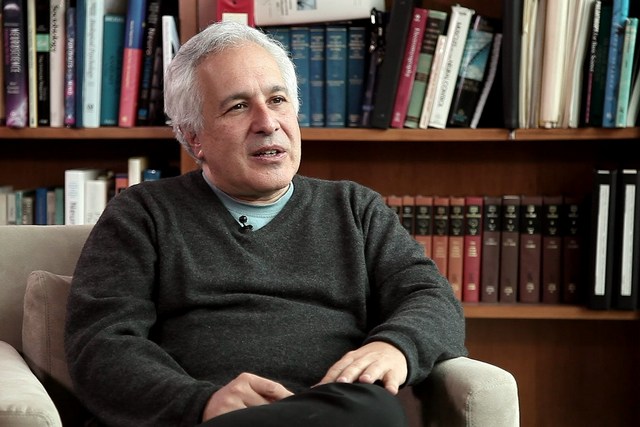
Oncologist Justin Stebbing on targeted therapies, side effects of chemotherapy and how multidisciplinary approach can help to improve survival of patients with cancer
videos | June 25, 2020
What methods are used to treat cancer? How do targeted therapies work? How can we better personalize treatment? These and other questions are answered by a Professor of Cancer Medicine and Oncology at the Imperial College London, Justin Stebbing.
I’m going to talk about personalized therapy, which means different things to different people. But what personalized therapy means is taking an individual, in my case, an individual affected by cancer, and treating them not like a conveyor belt, not like a car factory, but treating them according to their individual requirements. That means treating the right person at the right time with the right cancer with the right treatment.
Let’s deal with each of those four components. What do I mean by the right person? It depends on what the person wants, whether they want to get better or not, whether they are old or young, fit or unfit, where they live, what their social circumstances are, and what their genes are that may have contributed to the development of cancer. ‘At the right time’ means that we try to diagnose cancer earlier and earlier, and we’re using blood tests and imaging techniques to do that. People often ask me, is cancer curable? Well, most cancers are curable if you detect them early enough, and when common cancers such as colon, breast, prostate or lung cancer spread, we no longer consider them curable. In those cases, we aim to make people live with them for as long as possible with a good quantity and quality of life.
The right treatment means so many different things to so many different people. I like a multidisciplinary approach where decisions are made in conjunction with pathologists and radiologists, surgeons, radiotherapy specialists and drug specialists such as myself. We’re understanding whether to use hormonal therapy, chemotherapy, immunotherapy, radiotherapy or surgery when and how and in what order, and when we understand that better using a multidisciplinary approach, we’re treating people better.
But people need to help themselves with the right diet, they need to stay fit and strong and well-motivated as well.
When cancer spreads, what we need to do is control those cancers by understanding the signalling pathways in those cancers using targeted therapies as well. What the targeted therapies do is they target the proteins that are made within cancer cells as a result of mutated or fused genes. The drugs bind to those proteins that are unique to cancer cells, leaving normal cells alone, so side effects are much less. They can still occur, but they’re much, much less. So the way targeted therapies work is they’re often small molecules or antibodies that focus just on the changed genes within cancer cells. They’re much more selective, they’re much more suitable, but you can’t give them to all cancer patients: you need to test the cancer to see if it’s the right treatment for those patients.
But sometimes the targeted therapies don’t exist, or they’re not available because of things like cost, or we know that genes aren’t working, but the targeted therapies have been used and have stopped working. Sometimes, we need different approaches, such as chemotherapy, which still works despite its side effects, such as fatigue, bone marrow suppression, hair loss and mouth sores. One of the problems with chemotherapy is it can kill all rapidly dividing cells. That’s not just cancer cells: it could be hair cells, gut cells, nail cells, or skin cells, which is why it has a lot of side effects. For example, bone marrow cells divide rapidly to make red and white cells, and that’s why chemotherapy can lead to anaemia or neutropenia, which leaves people at risk of infections because the white cells are eradicated.
There’s no one individual who created personalized therapy: it’s a movement which has come about as we’ve understood that you can’t treat everyone in the same way.
A one-size-fits-all approach doesn’t work, a bit like if you go to a clothes shop or a shoe shop, you’re not going to buy a pair of shoes that someone else bought: you want the right shoe for you that fits your foot. Or think of a key to open the door: you need the exact key that fits in the exact lock.
The personalization of therapy, targeted therapy, and precision medicine have been coined by various people over the last few years. What it means now is treating people using molecularly targeted approaches. As a clinician scientist, I believe that’s the best way forward for our patients to improve survival.
So, my research into this therapy regards genes inside cancer cells called kinases. Kinases turn on cancer cells, and so we’re looking at different cancer cells and ways of inhibiting those kinases to turn them off. Most oncology drugs focus on turning off genes that are turned on in cancer cells, and by understanding those genes better, we can make treatments more precise, more targeted and more personalised and treat people better so they live longer.
The future directions and research is really understanding at many levels how cancer cells change over time. By understanding cancer stem cells and the network effects, understanding the way gene dysregulation of not just cancer but the connective tissue within cancer, the blood vessels, the surrounding stroma and the microenvironment contribute to the survival of cancer, by understanding those genes better, we can understand how better to turn them off to improve survival.