Contracting human muscle tissue created
New eLife paper explains how artificially generated human muscle cells will help develop novel treatments
news | February 12, 2015

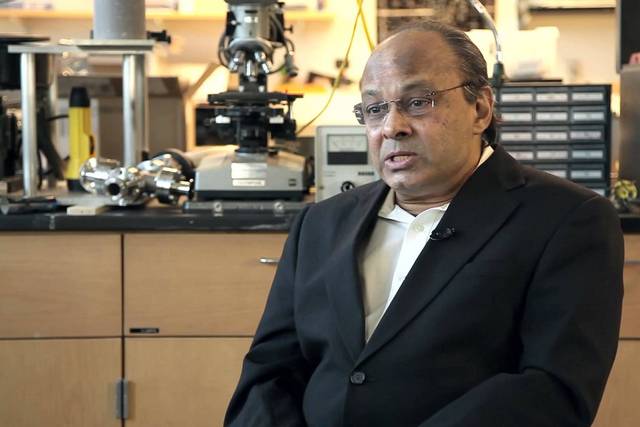
On January 9, 2015 eLife published a paper “Bioengineered human myobundles mimic clinical responses of skeletal muscle to drugs” about creating contracting human muscle tissue in a dish for the first time. We have asked one of the authors of this research, Prof. Nenad Bursac from Duke University, to comment on this work.
The Study
We are the first group that succesfully generated contracting muscle microtissues using human muscle cells. We achieved that by carefully optimizing culture conditions including methods to expand and then to culture cells in a three-dimensional hydrogel protein matrix. By doing so, we made the first human skeletla muscle microtissue model that in response to electrical stimulation generates classical muscle contractile responses (twitch and tetanus). We have also shown that these miniature engineered muscles (that we call “myobundles”) contract in response to acetylcholine, a chemical that is naturally secreted by neurons in our body to activate muscles and induce motion, for example. We demonstrated reproducibility and robustness of the approach by generating functional myobundles with similar properties from 10 independent donor muscle samples. We further went to show that myobundles have intact signaling characteristic of native muscle and respond to a diverse set of drugs in similar fashion to how human muscles do in clinics.
This progress finally enables researchers in the field to study human muscle physiology and drug responses in a dish rather than only being able to look in biochemical outputs (gene and protein expression). As we can get more than 1,000 myobundles from a single small needle muscle biopsy we now have a platform to study beneficial (or toxic) effects of multiple drugs on the muscle from the same patient, opening doors to novel drug development studies and design of personalized therapeutics. This is exactly what “precision medicine” is all about. For example, with clinicians from Duke University we have started obtaining muscle biopsies from patients with a specific muscle disease. We are generating myobundles from these biopsies and are now working to validate that the results seen in clinics are the same to those we see in the lab – importantly, on a patient-per-patient basis.
Background
Future Direction
Future research in this field will be geared towards modeling of human muscle disease in a dish and combining multiple human microtissue systems (e.g. muscle, heart, liver, gut, fat, etc) into a single platform, called “body-on-a-chip” that would hopefully be more predictive then animals are when testing the drug safety and efficacy. As I previously mentioned, such platforms will be made using cells from a single patient, thus allowing precision medicine applications and drug treatments tailored to single individuals (i.e., “you-on-a-chip” application) rather than average populations, as has been the long-standing practice.
If you would like to contribute your own research, please contact us at [email protected]