Geographic Variations in Medical Practice
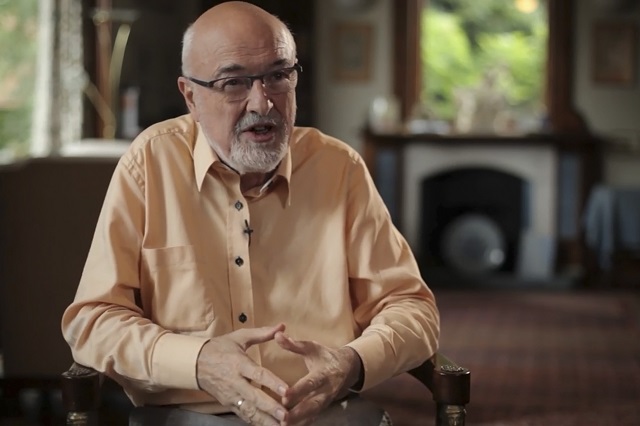
Professor David S. Jones on local standards of healthcare, practice patterns, and Medicare
videos | July 24, 2015
Why is there a 100% variation in Medicare spending per patient in different states? How do patient preferences account for surgical rates in a region? What can we do to ensure the practice is fair everywhere in the country? These and other questions are answered by Harvard Medical School A. Bernard Ackerman Professor of the Culture of Medicine, David S. Jones.
So if you are someone in the United States or in any other country in this world, who has the misfortune to have a heart attack – what happens to you depends a lot on where you happen to have that heart attack. In the city where I live, in Boston, your treatment can depend on which hospital the ambulance takes you to, which doctor happens to be on call that night and what kind of insurance that you happen to have.
You can see these kinds of practice variations everywhere you look. Practice variation varies from city to city, from state to state within the United States and from country to country worldwide. Now this isn’t variation that’s being caused by variations in the underlying burden of disease. If you control for the rates of heart attacks and if you control for the rates of the health of the population, you’ll still see this kind of practice variation. And because of that, researchers have identified this as the problem of unwarranted variation in medical practice – variation in practice that doesn’t make sense. Not that you can’t explain that, but that ought not to exist.
And so since the 1960s, with the increased attention since the 1990s, since the cost of healthcare has increased dramatically, researchers have really tried to get to the bottom of this question of unwarranted variation to try to understand why is it that medical practice varies so much from place to place. And there are several broad styles of explanation that have been suggested to account for this kind of unwarranted variation.
And so it’s clear that the financial structures at healthcare system and reimbursement clearly account for some of the variation that you see from place to place in medical practice. But they don’t account for all of that, and what researchers have done to show this – is they got the groups of patients who all have the same kind of insurance and who are all exposed to the same kind of financial systems within a healthcare system. So in the US you can look at patients who have Medicare – this is everyone over age 65, they all have government-based health insurance that reimburses doctors roughly, not exactly, in a roughly equivalent way. And if you look at variations in Medicare, you will see huge demographic variations. The average Medicare spending per patient in the US varies from as low as 5000$ to 7000$ per person per year in some parts of the country to as high as 13000$ to 15000$ per person per year in other parts of the country. A 100% variation in cost affecting variations in practice within a pool of people who have the same insurance and same financial incentives.
So the question is why. Well, economists have offered solutions. Some economists have said this is a problem of supplier-induced demand. If you train doctors, if you train surgeons, then they do what they have been trained to do. So if you have one state that has a thousand surgeons and one state that has ten surgeons, there will be more surgery in the state with a thousand surgeons, than there is in the state with ten surgeons. And that’s likely true, but again, that’s not a full explanation.
Psychologists have looked at this and said there are a variety of psychological factors that figure into this. Some of it is the influence of local personalities. If you have a major academic medical center that has a charismatic chairman of surgery who has trained generation after generation of residents to practice in that particular way and those residents mostly end up working within 15 miles radius of that medical center, then you will see an effect of that individual charismatic surgeon on practice patterns in his area.
Some of it is also peer pressure or local standards of care: if you practice one way, and everyone else in your community is practicing another way, over time it seems that people drift so their practice patterns become more like that in their local community. People are affected by the situation in which they live.
Patient preference might account for some of this, so if you live in an area where patients for whatever reason are averse to surgery you might expect to find surgical rates to be lower than they are elsewhere. Sometimes it begs a question: well, why are the patient preferences varying – it’s not like patient preferences come from heaven or something, there are reasons why patients have preferences.
Usually it has something to do with what they have been told by doctors or what their past experiences with healthcare are. That’s right, patients’ preferences vary from place to place. Some countries have cultures that are much more interested in aggressive intervention, other countries aren’t so interested in that, and you can see that changing culture’s hyper personality type or patient preferences playing out in how medical treatment is done.
And so the researchers have looked at this question of unwarranted variation, and they have found a wide range of factors. No single factor accounts for all of it; if you try to explain high rate of procedure X in one city, there might be 4-5 factors that explain it, if you try to explain high rate of procedure Y in a different city, there are likely to be 4-5 different factors that explain it.
The causes of variations themselves vary in a way that presents an interesting puzzle for researchers, but a really complicated problem for policy makers.
So the question that has always come up is: we know that variation exists, we have very good knowledge of the types of things that cause variation, so what can we do to get rid of it? What can we do to ensure that the practice of medicine is on as rational solid basis as possible?
And it is really difficult, because the causes of practice variation vary, the policies will need to vary as well. There are some low-hanging fruit: if you get rid of fee for service, you get rid of whole series of financial incentives. If you do very close monitoring of outcomes, you can identify people who are doing things that are providing high-value care. If you educate patients better, you can likely standardize the kind of preferences that patients have, then you bring with them into the clinics and the hospitals. There are many things you can do, there is not going to be one perfect solution, but over time you should be able to chip away at this problem.
Now if you look at this at a global scale, the kinds of disparities that exist are even vaster. So you might say, well, rates of bypass surgery vary by a factor of 2 or 3 in different regions of the USA, they vary by a factor of 6 to 10 between different countries in North America and Europe, and they probably vary on a scale of a hundred or a thousand on a global scale. Pick two countries: Germany and Mexico. They have very similar rates of coronary artery disease, the angioplasty rate in Germany is a hundred times higher than it is in Mexico. It’s not because of the burden of disease, the burden of disease is the same. There is something about the structure and the function of healthcare systems in Germany and Mexico that makes the procedure very common in Germany and very rare in Mexico.
Trying to figure out the causes of this global variation are similar to trying figure out the causes of more local variation – everything is just on a bigger scale. And trying to figure out policy solutions is a much, much more difficult task, because the scale – the size of disparity, the number of people are involved are much, much larger.

Well, the question is: does it apply to every treatment that exists? There are huge disparities that are out there for every treatment that exists: if you are in Germany, if you are in England, if you are in the US, you have much better access to treatment for cancer, for heart disease, for diabetes than you do if you are in Mexico, in Brazil, or India, or China, or even more so for the poorer countries worldwide.
Should the rich countries in this world be making the same kind of commitment to global health equity for all treatments that they are for AIDS? From the moral point of view the answer seems like an easy one: well, of course they should. From a practical point of view it’s a much, much more difficult question.
So when you look at these huge disparities that exist between countries on a global scale in terms of access to a treatment for cancer, or heart disease, or the other leading causes of death, there are many different factors that contribute.
The one that gets the most attention is financial. Treatments for heart disease are expensive, treatments for cancer are expensive, and many countries just don’t have the national healthcare budgets that would cover this. That was initially a problem for AIDS, when AIDS treatment was 10000$ per person per year, that was very hard for countries in Sub-Saharan Africa to manage. Well, what happened? Two things happened: first, the cost of treatment has dropped enormously – it is now a 100$ per person per year. And wealthy donors, both individuals and national donors from countries decided that they would make a commitment to making this possible.
Well, could something happen with the cancer or heart disease, cost amount would not be so valuable, the motivation of donors, individuals and government is going to vary, I think, depending on a disease and the social meanings of this disease. And then there is also a question of capacity. It’s one thing to try to get medications into the hands of patients every day so they could take them, but if you want to provide people access to radiation therapy – that’s complicated, because they need to build machines and infrastructures, that are likely to be built in cities. And how would you do with countries that have majority of rural populations? Or if you want to get people access to surgery – again, that’s complicated, because you need an elaborate hospital infrastructure, and you need a blood supply, and you need all sorts of surgeons, and instruments, and sterilizing equipment to make these things work.
Different kinds of treatment are more or less complicated, and sometimes the problem is not necessarily inside the healthcare system, as outside the healthcare system.
I was in India recently interviewing cardiologists and cardiac surgeons about the prospects for the future of aggressive cardiac treatment in India. Now, India is a country that has more heart-attack deaths than any other country in the world. Not the highest rate, but the highest whole number of deaths. And very few people have access to advanced cardiac care.
I was talking to one of the cardiologists, and he said: look, we could open up an angioplasty center in every hospital in Mumbai or Deli, but there is no ambulance service. If someone has a heart-attack at home and they call an ambulance, there’s a chance that they might get someone to come pick them up, but because of the traffic it will likely be an hour before an ambulance arrives at their house, and another hour before they get to the hospital. If you want to make this thing work like it works in Boston, you will need to totally re-do the urban infrastructure of major cities in India, and this is a problem in many countries worldwide. And so some of the challenges really do feel insurmountable.
So going forward for people who are interested either in just improving the health and access to healthcare of these populations worldwide, or for people who are interested in this higher ideal of global equity for health outcomes, we really need to do some seriously creative thinking to try to figure out not just these financial obstacles to healthcare, but deeper structural barriers that will make it hard to allow every person on the planet to get the full potential benefit from healthcare.