Post-Traumatic Stress Disorder
Neuroscientist John Krystal on flashbacks, relative merits of different treatments, and brain tissue collection
faq | August 15, 2016

After people are exposed to very difficult experiences in their lives, they often have difficulties related to that exposure. This is called Post-Traumatic Stress Disorder, or PTSD. The people may notice that the thoughts or the memories of the traumatic event intrude on their thinking and interfere with their concentration during the day and that those thoughts about the event appear as dreams at nighttime. They may have daydreams about the event, and those daydreams can be so vivid that the person may feel that they are actually reliving that experience. Sometimes those reliving experiences are called flashbacks.
Flashbacks
The flashbacks vary, and they depend on the nature of the trauma. People who have flashbacks usually have the most severe PTSD symptoms. One feature of the experience is these intrusive memories and thoughts about the trauma. Those memories are sometimes sad experiences, such as seeing people die or seeing bad things happen to other people. Other times, they are very frightening memories because, generally, at the time of traumatization, people are very frightened; something very scary is happening.
So after the event, they may find that, when the memories come up, they make the person feel guilty, sad, or frightened. And even not specifically remembering, encountering anything that reminds the people of the trauma may acquire the ability to make them feel very tense, anxious, and defensive. In other words, for example, we often see in soldiers who come back from combat that they are generally wary and uncomfortable in situations where they feel vulnerable. So they may always sit watching the door, or they may be very cautious about being in crowded places. In addition, their arousal system can be very activated; they can feel tense, jumpy, and anxious, and they can have anxiety attacks. And they can have those experiences even when they’re not thinking about the trauma in a specific way.
Usually, the flashbacks only last a short time, maybe a minute or two. But when people are having a flashback, sometimes they don’t respond well to environmental stimulation. However, if you’re talking to someone and you can reach out to them and engage them in the discussion when they’re having a flashback, sometimes you can make it shorter. There are also medications, such as Valium, that people sometimes take to help them to relax.
Symptoms and Diagnosis
In this way, some of the symptoms are intrusive thinking about it, hyperarousal, and possibly shame or guilt as an emotional reaction, or feeling emotionally numb or mechanical in one’s daily life. In other words, people might not feel that they are experiencing the full range of emotions, particularly emotions like pleasure. There’s also an additional defensive attitude, conditioned emotional responses such as anxiety, and depression-like symptoms. Those are the general groups or clusters of PTSD symptoms.

There are certain diagnostic criteria, and if you have enough of the symptoms, you can meet those for PTSD. However, there are a lot of people who don’t meet the diagnostic criteria because they don’t have enough of the symptoms but who still have some post-traumatic stress-related symptoms. And sometimes, even if you don’t fully meet the diagnostic criteria, you should still get help because you could need help with those particular symptoms.
History of Research
What’s interesting is that researchers have inferred from literature, going back all the way to the Iliad and other historical sources, that people were always aware that after going through terrible things, individuals would have strong emotional reactions. However, as a formal diagnosis, the label “Post-traumatic stress disorder” didn’t appear until 1980, which is, in terms of the history of psychiatry, extremely recent for a major diagnosis to appear.
In the American Civil War, the Crimean War, the First and Second World Wars, the Korean War, Vietnam War – in all of these, at the beginning of the conflict, the physicians, the psychologists, or the mental health practitioners seemed like they had forgotten all the prior experience from all the prior wars. And for each of these, at the end of the war, there was an elaborate level of clinical expertise appropriate for that period in history.
During the First World War, there was a lot of work on what was then called “shell shock” or “traumatic neurosis.” In America, there was a psychiatrist, Abram Kardiner, who wrote a lot about it, and Sigmund Freud wrote about it around the end of World War One and into World War Two. When people see a lot of trauma, there is always elaborate understanding, but somehow, maybe not intentionally, there seems to be this trend in society that after major periods of trauma in the past, knowledge of that trauma and its importance can fade a bit.

Soldiers during the Battle of the Somme in World War One, many of whom experienced “shell shock”
However, after World War Two, there was a classic study of pilots done by doctors Grinker and Spiegel that was a wonderful descriptive work of Post-traumatic Stress Disorder. And in the late 1950s and early 1960s, there was a group of psychiatrists who worked on PTSD. Robert J. Lifton was one, and my father, Henry Krystal, who had worked with Holocaust survivors of the Nazi death camps, was another. After that, there was a whole group of people, including Matt Friedman, Terry Keane, Dennis Charney, and many others, who worked with the Vietnam veterans, as well as many other researchers, such as Leo Eitinger and Lars Weisaeth, from all around the world. This is a field, a problem that affects every country, and in every country, there are people who study it and have made important contributions to this kind of work.
One important researcher of PTSD was my father, who passed away last year and who was a survivor of Auschwitz, among other camps. When he came out of the camps, he decided he would try to go to medical school and ended up moving in with an aunt in the United States. He graduated from medical school and went into psychiatry, and started to work with other survivors of the Nazi death camps. He was evaluating people, other survivors, for disability pensions, and he did a very careful study of those survivors, which was one of the very early descriptions of the syndrome of Post-traumatic Stress Disorder. He was a psychoanalyst, so he went on to try to develop psychotherapeutic approaches from a psychoanalytic point of view that integrated aspects of behavioral psychology, cognitive neuroscience, and other fields that he was interested in. In this way, he developed some improvements in therapy that helped people with PTSD, who often have difficulty articulating their emotions and feelings.
You Can’t Categorize Trauma
One of the important results of such cultural experiences as war and other major upheavals is that we’ve begun to extend our appreciation of the kinds of situations that can cause trauma – trauma in adults, a trauma in children – things like physical and sexual abuse, witnessing terrible events and so on. So the reach of PTSD in society is much greater than mere populations like soldiers, where PTSD is often a relatively visible problem.
Something that is often underappreciated is that the issue with PTSD is not so much how bad the event is from an external point of view. Although there are efforts to try to standardize or to narrow in some way the scope of events that would be truly traumatic, for some people, it’s the meaning of the event, not the severity or actual danger of the event, that causes trauma. There are situations, for instance, when people are extraordinarily reactive to something that seems benign. When that happens, it is usually because the people believe that their life as they know it is over, something fundamentally tragic and devastating has happened to them, and is perceived that way by them even though it wouldn’t be perceived that way by others.
It’s easy to get caught up in the labels of things, and for the purposes of this discussion, it might be good to even set the notion of PTSD aside from other kinds of stress reactions. But you can imagine, for example, how, for some people, if a romantic relationship breaks up, then for some period of time, that separation does feel like the end of their life as they knew it. So even if that event doesn’t trigger full-blown Post-traumatic Stress Disorder, clinicians have learned to respect the impact of these situations on people’s lives and try to help them through whatever adjustment process they go through.
Treatment Through Psychotherapy
The most common ways that people are treated for PTSD are either some form of psychotherapy or counseling, on the one hand, and, on the other hand, some kind of medication. Now, one of the things that are no longer done is forcing people who are very upset and preoccupied with their trauma to tell their traumatic story over and over again right away, right after the trauma. People used to use this technique — traumatic debriefing because they thought if they could just get people who were acutely traumatized to tell their full stories, those people would feel better. But it was discovered that pushing people too aggressively to tell their full stories right away actually tended to reinforce the memories and the negative reactions to the trauma.
In progressive exposure, you start with the most gentle, least upsetting trauma-related memory, and you learn to relax and not be upset by it. Then you go to the next more upsetting thing, and the next, and so on. In cognitive processing therapy, there is some of that as well, but there is also working with patients to try to correct any inaccurate ideas, assumptions, or conclusions that they may have drawn from the traumatic experience. For example, a woman who has been sexually assaulted might think that all men are dangerous. In fact, only some men are dangerous, and becoming comfortable with putting the traumatic ideas in a more adaptive context is an important part of cognitive processing therapy. Eye movement desensitization, in turn, has elements of the other two therapies and also has a third component, whereby, essentially, the therapist distracts the patient by having him or her move their finger from side to side and focus on the finger moving back and forth. This focus on the irrelevant finger is a technique that helps some people relax in the context of traumatic memory.
Then there are a variety of other techniques that people are beginning to explore. For instance, there are some mindfulness-based therapies, which are ways that people learn to relax and manage their emotional reactions, and many other therapies as well. Overall, people find these both comforting and helpful. Another aspect of all of these therapies is that they also have an educational component.
In the days before Post-traumatic Stress Disorder was understood, there used to be people with PTSD who presented for treatment but who had no idea what was going on and thought that something was the matter with their heart, their intestines, or their head, or that an unknowable bad thing was happening to them and they didn’t understand it. And that in itself, the lack of understanding, was very distressing and a big problem. So for those people, when doctors explained to them what Post-traumatic Stress Disorder was and how the symptoms that they were experiencing were both common and treatable – just that understanding often helped people feel a bit better.
Treatment Through Medication
The strength of the evidence supporting psychotherapy is, at this point, better than that supporting medication. However, there are a number of medications that have been tested and found to be helpful. In the United States, the two validated medications are both antidepressants and work in very similar ways. They’re called Selective Serotonin Reuptake Inhibitors, or SSRIs, and one of them is Sertraline, and the other – is Paroxetine.
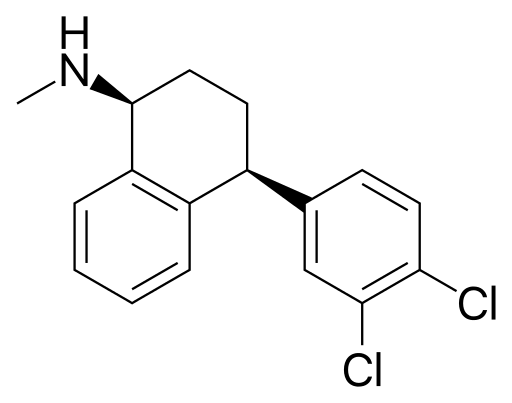
Skeletal formula of Sertraline
These are standard antidepressant medications developed for the treatment of depression. They work somewhat with people with PTSD and help many of them. There are also many related medications that, to the extent that they’ve been studied, have evidence supporting their effectiveness. These are the Serotonin and Norepinephrine Reuptake Inhibitors, an example of which is Venlafaxine. There’s a nice study of Venlafaxine as a treatment for PTSD, as well as a few studies of older antidepressants, such as Desipramine, Imipramine, Amitriptyline, and Monoaminoxidase Inhibitors that are widely prescribed in Europe and other parts of the world.
There are also medications that emerged out of clinical practice and for which the strength of the evidence supporting their prescription is not very high. These include second-generation antipsychotic medications, benzodiazepines like Valium, anticonvulsants like Lamotrigine, and a typical antidepressant called Trazodone, which is often prescribed for sleep. These medications serve to reduce anxiety and hyperarousal and tend to make people feel a little bit more in control of their emotions, helping them to sleep a little bit better. Overall the medications seem to be about as effective as psychotherapy, so what you see in clinical practice in a lot of places is that, most commonly, people get psychotherapy and medications together if their symptoms of Post-traumatic stress disorder are sufficiently severe.
Brain Tissue Collection and SGK1
Recently there have been a lot of breakthroughs in PTSD research. A really exciting one was made by Dr. Ronald Duman at Yale, working with the first brain tissue collection in the field of PTSD. In other words, from a medical point of view, if you have a problem with your kidney, chances are that the doctors who are treating your problem know a lot about the kidney because they’ve studied the biology of the kidney in the context of all the illnesses that affect it. They look at the actual cells of the kidney, and they figure out what’s going on with them.
That has been an extremely powerful approach in neuropsychiatry as well, in some cases: scientists have learned a lot about the biology of Alzheimer’s disease, Schizophrenia, or depression, from studying the post-mortem brain tissue. But the brain tissue of people with Post-traumatic Stress Disorder has never been collected before since it’s a relatively small field of research.
With support from the Department of Veterans Affairs, the first brain tissue collection of PTSD got started in 2016, and the first study from that brain collection came out; as expected, it turns out that previous ideas about Post-traumatic Stress Disorder are partly right and partly wrong. The brain tissue from PTSD is telling us some very exciting things, and there’s one story that illustrates perfectly the kind of thing that comes out of it.
In Post-traumatic Stress Disorder, the executive control of emotion, our ability to calm ourselves down after we encounter something scary in the environment, is affected. Some of the ways that we use to calm ourselves down are distracting ourselves or telling ourselves, “It’s actually ok, don’t worry,” and the part of the brain that’s doing that calming is the frontal cortex. In the Brain Bank, there is now tissue from the frontal cortex in PTSD, and Dr. Duman looked at the level of something called mRNA. MRNA is the product of genes that code for proteins that make up the brain. It turns out that one of the mRNA levels that was particularly low in the frontal cortex of the PTSD brains was something called SGK1. SGK1 is not something that anyone has ever studied in PTSD before, but it is a little bit connected to Cortisol, which is a stress hormone that is released when people are under a lot of stress.
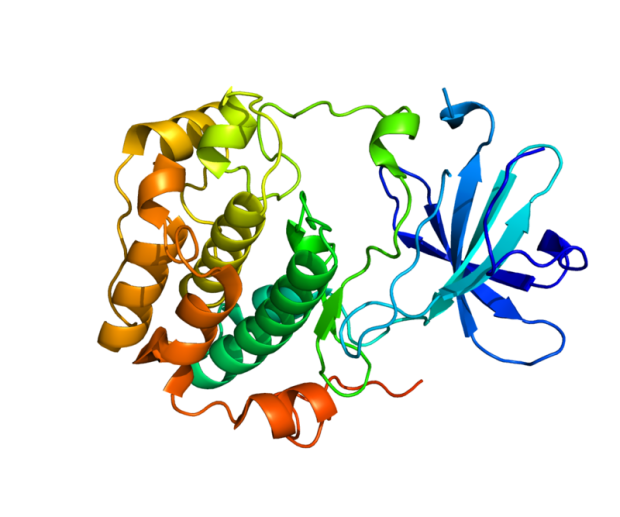
The structure of protein SGK1
To try to understand what low SGK1 levels might mean, the first thing he did was to stress something else, and the first thing he found was that if you stress animals, then the SGK1 level in their brain goes down. And then the second thing he did, which was really interesting, is that he asked the question: “Well, what happens if you just happen to have a low SGK1 level? Does a low SGK1 level do anything?” So he created an animal that has low SGK1 levels in the brain, and those animals tend to be very stress-sensitive, like they already have PTSD, even though they were never exposed to stress. Okay, so low SGK1 in PTSD, low SGK1 in stressed animals – low SGK1 makes you more stressed.
So what would happen if you could raise SGK1 levels? Dr. Dumin used a technique to do just that and to then protect those levels from dropping. It turns out that if you do that, animals don’t get PTSD. In other words, they become very resilient to stress. That suggests that maybe one of the strategies that should be followed in PTSD research is to look for medications or maybe even other kinds of methods, like exercise, that can raise SGK1 levels.
Alternate Areas of Research
So that’s one completely new strategy of going from a molecular signal in brain tissue all the way to a new treatment that’s never been tried before in PTSD but which we can now do. There are also a variety of other exciting areas: from brain imaging scans, we are learning about the circuits that seem to be implicated in Post-traumatic Stress Disorder – how the circuits go awry, how they are related to symptoms of PTSD (this is from functional neuroimaging scans); and from genetic studies, we are learning about gene variations that may make people more sensitive to stress.
For instance, early on, there was work that suggested that a serotonin transporter gene made children more sensitive to early childhood maltreatment and made them more likely to develop symptoms of PTSD and depression. And this kind of work is going on in children, it’s going on in adults, and there’s now another gene linked to Cortisol called FKBP5 where alteration may be relevant to PTSD.

So one of the questions has been: “What kind of treatment can be developed that isn’t aimed at targeting just the symptoms of PTSD, but also aimed at helping the brain to regrow these synaptic connections between nerve cells so that the circuits could work more effectively in regulating mood?” And interestingly enough, Dr. Dumin’s laboratory discovered that if you give a single dose of Ketamine to the animals, the circuits actually do rapidly regrow these synapses.
It’s an incredible thing – you look under the microscope, and you can actually see these new so-called “dendritic spines” growing within an hour or two of taking a single dose of Ketamine. Afterward, Ketamine was given to people with PTSD, and they showed some signs of clinical improvement. This is another exciting area where treatments are being created not just because of what we observe in terms of the symptoms but also in terms of how the brain circuits are working – a rational, scientific approach.
So there’s a lot of exciting research going on from the biological point of view, there’s a lot of work to continue to validate and disseminate the psychotherapies, there’s work on genetics, and there’s work to try to develop medications as well. A lot is happening that has the potential to change the way we think about things related to PTSD.
Edited by Alina Shubina