Tissue Engineering Applied to Cancer
Biologist Ali Khademhosseini on tissue engineering, drug testing, and nanomedicines for cancer
videos | July 10, 2015
Why do we need human cancer tissue? How to study the effects that therapies have on different organs? How do nano medicines work? Full Professor of Medicine and Health Sciences and Technology Harvard-MIT, Ali Khademhosseini, talks on applications and challenges of cancer tissue engineering.
Cancer is one of the biggest problems facing our society right now. Pretty much everyone knows someone who has cancer. And it’s a devastating disease, because it causes, in often cases, people going through lots of hardship, and causes death to people who are really at early stages of their life. When you think about major challenges that are addressing our society, cancer is one of the major ones.
So how do we actually apply some of the technologies like tissue engineering to cancer? Well, I think there’s a few different ways we can think about this. Tissue engineers, of course, what they’re doing is in many ways what tumors are doing. Tissue engineers try to make new tissues, and we want these tissues to be very well vascularized. And really in some cases this is what tumors do. Tumors basically are making new tissues and they want it to be very well vascularized so they can grow. So in many cases we are trying to use the same kinds of principles to come up with new tissue. Of course, the end goals are very different, and in our cases we want to use cells that are therapeutic, but in cancer cells those are uncontrollable cells, and they grow indefinitely, and wind up being big problems.
One of the ways in which tissue engineering and cancer can interact is through using tissue engineering to understand cancer at the biological level and trying to understand how things like tumors are formed, and how we can use three-dimensional constructs to understand cancer cell – normal cell interactions, and how cancer cells actually grow, and how cancer cells go into the bloodstream and metastasize to other tissues. And there are some of the things that, by having proper three-dimensional constructs, three-dimensional ways in which you can culture cancer cells, you will be able to answer them and study cancer much better. And this is one of the first examples of how technologies that have been applied to tissue engineering can be applied to understanding cancer.
Imagine that you have a therapy, let’s say, a drug that you want to test. If you can put this drug in mice and rats with sometimes mice’s and rats’ tumors you get often a solution. But if you take the same drug and you test in on human cells, in even two dimensions maybe it works, but if you take the same thing and put it in a tumor that is a three-dimensional environment, then it doesn’t work. So if we can try to predict this kind of behavior by having in vitro systems and tissue culture methods where we can grow these tumors and have them be predictive of what happens to the drug, then it would be very beneficial.
Or imagine if you have some kind of therapy that is an imaging therapy plus a radiation therapy, where you want to test that. Well, if you have a kind of physiological method, where you don’t necessarily use mice and rats, which are very small, maybe you can image them easier; if you have a piece of tissue that is more representative of human tissue and you can now image the tumor, and you can use radiation, and test those approaches in a more controlled human model, then I think you have more advantages here.
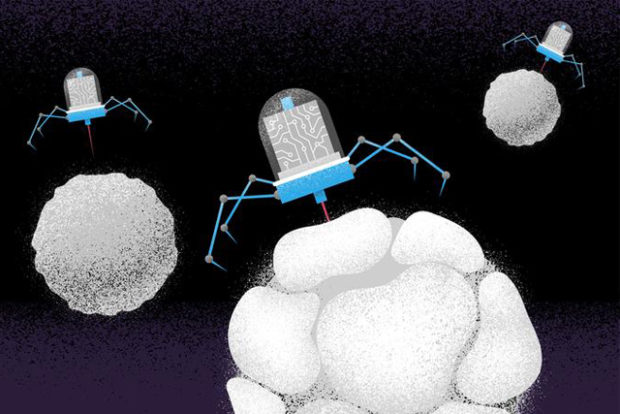
Those are some ways in which you can use cancer models and tissue engineered cancer models, and then test therapies. Another one that’s we think is very interesting and very futuristic is to test engineered tumors and test targeted therapies. So there’s a whole emerging area of trying to use nanotechnology, and specifically nanoparticles that have drugs to treat cancer. So the idea here is that you can put drugs inside very small particles and you can inject them. And these nanoparticles, if you design them properly, they can go circulate in your blood, and when they see tumors or cancer cells, they can attach to those cancer cells, and release their drug and kill only the cancer cell and not the other cells that are not cancerous. So this is a concept that is very powerful, and people have tried to make this work.
But some of the challenges are that we don’t have good cancer models. A lot of times some of these things work in mice and rats, but when we test them in humans, we don’t get the same targeting effect.
If we have a properly engineered tumor, then we can test these drugs that are targeted to only affect cancer cells.
And we can test them in an engineered tumor that has the right blood vessels, so we can literally have these things go through the blood vessels that we can engineer in these tumors. And once they’re going through the blood vessel we can test whether the right kind of a nanoparticle interacts with the right kind of a cell, and whether it kills only the cancer cells and not other cell types. So these are some examples of how cancer and tissue engineering can interface.
Of course, there is a lot of other applications as well that are relevant for pharmaceutical industry. For example, every time right now we want to make any kind of drug, including cancer drug, it costs about 1.4 billion dollars. This is because what people do is they start with a lot of different chemicals, and then they test them in these little dishes with cells, and then you start doing your animal experiments, and from the ones that are working in animals you start doing human trials. And this is a huge costly endeavor, because many of the ones that you test actually don’t work. And this is why cancer therapies that get approved are very rare.
So what we can do with some of these technologies again is that we can address it to that problem. Instead of using mice and rats, we can take all these candidate drugs and then be able to test them on human tissues with human responses and then, before they go and get tested in clinical trials, we can have a much better predictivity of what happens.
In most of the cases I talked about, you only have a tumor and you test it on a tumor. But now imagine, instead of just having a tumor, you can connect your tumor to a heart, to a liver, to a lung, to a bone, to guts, to other things. And you can start making human version of a response in a dish. And so then you can see whether your cancer drug not only kills the tumor, but it will have liver toxicity or cardiac toxicity. And you can potentially see all those responses in a tissue-engineered constructs that can be applied to this cancer problem.

So they would not be a functional human, in the fact that they wouldn’t have, let’s say, a nervous system and it wouldn’t have arms and legs or anything, but it would simply be a way of having the right kind of interconnections between the miniaturized tissues so that you can have this. And this is a very powerful concept, because now you’re starting to get to processes that you can see their complexity in biological systems that you would not be able to capture in a single dish, single cell type cultures that are happening now all over the world in all these drug study experiments. And I think PhaRMA and other regulatory bodies are seeing this as a huge opportunity to be able to make the next innovation and coming up with new drugs that could be relevant to cancer as well as many other types of problems that are out there in the medicine.
With respect to tissue-engineered tumors, the way they are often made is they are made from cancer cells that are isolated, let’s say, from tumors. They’re made from the same cells, and they often grow into some kind of a structure that mimics many aspects of the natural tumors that exist in the body. Now people are starting to see that, based on how you engineer these, you can start getting more and more of the functions of the real tumor. So, for example, in the real tumor you have leaky blood vessels. That’s why if you have a drug therapy, sometimes it goes well in the tumor. Nanoparticles and things actually go in the tumor well, because of the leaky blood vessels. So in some of these engineered systems you can get those kind of properties. You can get tumor cells that actually come out and go to other places in the body and metastasize. And you can try to recreate some of those aspects in some of these engineered tumors.
So I think there are particular aspects that we can recreate, and one of the questions, of course, is how well do you need the tumor to behave to be able to see the effects that you want. And I think in some cases it depends on the questions you’re asking. If you’re studying and designing a drug that prevents metastases, and you can see that in your dish, and it prevents that, then you know that it’s a potentially good candidate for further testing. And I think in some of the cases your tumor needs to be only as good as your question.
So there are a number of potential challenges currently with this approach. A major thing is that many of the things regarding these multiorgan systems and tumors from tissue engineering applied to cancer are still at early stages. We still don’t understand a lot about how predictive they would be.
We believe that there’s a lot of opportunities to enhance our current systems, which are mostly based on two-dimensional cells, on two-dimensional dishes.
So we think that there’s a lot of opportunity. We don’t know how well we can make these. And that’s one of the challenges. We think that making these tissues itself is challenging enough. And now being able to make the tissues and link them together just technologically is very difficult.
Now also there are other challenges. For example, once you have an operating system, you often are dealing with things that are very small. And now in the same kind of analysis that we’ve developed to be able to analyze, let’s say, things from human serum and human samples, they simply don’t work, because we’re now dealing with small volumes of drugs and chemicals, and the things that are in the orders of microliters now instead of milliliters and larger. So we need to develop new toolset to be able to analyze these constructs in a way that is continuous. If you are doing something that is a twenty-day experiment, you need to be able to perform the experiment for the twenty days. So you need capability to make these tissues and visualize and analyze them for the duration of the experiments. And since these are different types of three dimensional tissues than what mice and rats are and what two dimensional cell cultures are, then the new toolset is being currently developed to really analyze them.