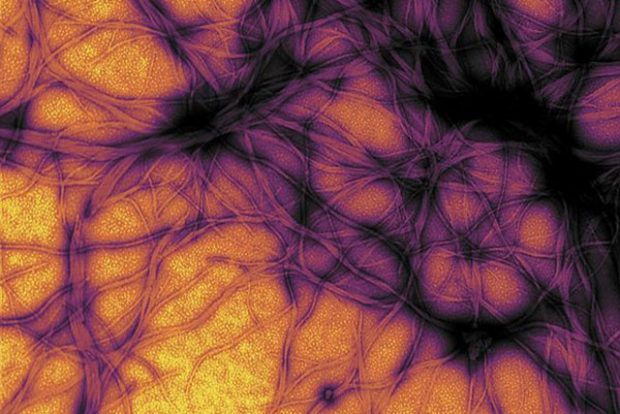
Brain Networks
Professor of Neurology, Neurosurgery and Biomedical Engineering at McGill University Sylvain Baillet on brain ...
In the late 19th century, neurologists emerged in France, Germany, and Britain who tried to characterize the phenomena of neurological disease as they saw it. They saw people who had muscle wasting, stiffness and spasticity of their limbs, disability of one kind or another, dementia, etc. So what we now view in the modern era as the core neurodegenerative diseases like Alzheimer’s, Parkinson’s and amyotrophic lateral sclerosis, all described in the late 19th century.
One of the features that neurologists were interested in is why people become weak. At that time, there was a relatively rudimentary understanding of the neuroanatomical basis of movement and voluntary movement. Largely, this emerged through lesions: during battles where soldiers were injured, people began to see that if you injure a particular part of the brain, you get a certain kind of lesion and a certain kind of disability. Strokes and brain tumours emerged, and people started doing anatomical correlations.
One of the questions that arose was if somebody’s weak and has muscle wasting, is that condition primarily a muscle disorder, or is it arising in the nervous system where the muscle, therefore, loses its connection? A particular neurologist, Jean-Martin Charcot, in Paris, coined the term ‘amyotrophic lateral sclerosis’.
‘Amyotrophy’ is wasting of muscle, ‘lateral sclerosis’ means that the lateral corticospinal tracts which are the long nerve pathways in the spinal cord which come from the motor cortex, these tracts are degenerate and become hardened or gliotic through scarring.
So, the term ALS or amyotrophic lateral sclerosis means both muscle wasting and damage to these corticospinal tracts.
We sometimes refer to ALS in the UK as motor neuron disease, which is not a particularly helpful term because there are many different types of motor neuron disorders. So, I think the term ALS is most helpful. It’s sometimes called the ‘maladie de Charcot’, and it’s sometimes referred to as ‘Lou Gehrig’s disease’ because, in the United States, a very famous baseball player developed ALS, so often it’s known as ‘Lou Gehrig’s disease’. Of course, what is happening here is that neurologists are describing clinical phenomena and then giving them a name, and the question then arises: is there one biological process going on that gives rise to these phenomena, or are there many things? To really try to understand that, you have to look at the neuropathology of the disorder.
Then, the era of genetics emerged, and in 1993, the first gene for ALS was identified. So it had been somewhat poorly described initially that this was a familial condition: Charcot knew that there were some families who had it, but mostly was thought to be sporadic, not really associated with any particular familial inheritance. But during the 70s, 80s and 90s in the last century, it became very clear that there were families with ALS. People collected these families together and, through classical linkage analysis using the genetic markers that were emerging at that time, began to map the genes that were associated with this disorder. The first gene on chromosome 21, superoxide dismutase, was identified: all mutations in this gene are responsible for about 20% of cases of familial amyotrophic lateral sclerosis.
Initially, people thought, well, SOD1 is the gene which is involved in oxidative stress and protecting the cell from oxidative stress, so clearly, that’s a very good candidate for something which might be related to neurodegeneration and ageing. Actually, it turns out if you look at mouse models of the disease where you put in a human mutation into the mouse, overexpress it to high levels, and the mouse does indeed develop degeneration of the motor system, actually, if you then supplement that mouse by crossing it with a mouse which is overexpressing SOD1 you cannot correct the disease. So, this is not a deficiency or a loss of function of SOD1, as far as we can tell.
So subsequently, in the last 20 years, we’ve looked at other families, and people have progressively identified other genes that are responsible. There are now between 20 and 30 credible genes which, if you mutate them, lead to ALS, which actually, to the neurologists in the clinic, looks rather similar, it looks the same. That tells you something very important: it tells you that the vulnerability to ALS, to motor neuron degeneration, arises not through specific pathways. You can organize these genes by function so that you can say, well, there are genes clearly involved in the regulation of protein homeostasis; that’s clear. There are other genes which seem to be involved in trafficking protein down the long axon, and there are other genes which appear to be involved in the way that motor neurons or neurons in general handle RNA, which is a very interesting whole area of motor neuron biology.
So how is it that these diverse pathways can converge on a disorder which looks absolutely the same in clinic effectively? It’s very very difficult. If I see a patient with ALS I can tell that’s familial by taking a family history, I can very rarely guess which gene it is going to be. There are some clues but it’s not reliable.
That means that the source of vulnerability here, the point of convergence biologically in ALS, is the system. The system is vulnerable; it’s vulnerable to a variety of different genetic insults. In fact, the majority of patients do not have a family history. Only about 10% of our patients clearly have an inherited disorder; the other 90% have a more complex disorder. That means that there are numerous upstream biological events which, if they occur in the right order at the right time in the right place, can trigger a catastrophic neurodegenerative disorder ALS in which patients will rapidly lose function.
So the corticomotoneuronal system is the architecture which connects voluntary centres in the brain with the centres initiating motor activity in the motor cortex, descending as the corticospinal tract, innervating lateral spinal motor neurons in the ventral horn of the spinal cord, various levels going out to muscle innervating individual muscle fibres through neuromuscular junctions. That is a complete architecture of a voluntary movement, and that is vulnerable. The question arises as to why it might be vulnerable and what are the sources of that vulnerability.
So, in ALS, typically, a patient will come to the doctor and report loss of function. The striking thing when you’ve seen hundreds of patients is that it always has a specific location, so a patient about 1/3 of the time will say they are losing function in one upper limb, and about 1/3 of the time, it’ll be one lower limb and the other 1/3 typically it’s the muscles of speech and swallowing. So, it raises the possibility, at least clinically, that this is a disorder which has a discrete anatomical origin, and it has a discrete origin in time. So, in time and in place, something is happening, which then triggers the disorder. If you then look at patients and follow them up, you don’t see random weakness throughout the body; what you see is a rather orderly progression of weakness through what one imagines to be specific networks within the motor system.
There are a number of different patterns. The most famous person with ALS is Stephen Hawking, who died last year. Actually, he was extremely unusual and atypical because he lived for 40-50 years after the diagnosis. It’s very, very unusual.
Most patients will succumb to their illness through respiratory failure within 2-3 years, and 10% of people die in the first year, 50% of people die by about 30 months after their first symptom.
So it’s an extremely aggressive process, and one of the key questions is how that process is progressing. If it starts in one place, how can it progress?
So, our current view of the origin of ALS is really a multi-step process rather like cancer. We imagine that patients are born with some genetic susceptibility, which may be very complex, or it could be very simple, one single gene mutation. On top of that, as the nervous system develops through numerous cell divisions and cell migration, errors may occur in individual pools of motor neurons, so-called somatic mutation or other genetic errors, and that can then seed an area which has a second hit, a second point of vulnerability. Then, as you get older, other pathways are failing the way that this protein is handled in a cell, perhaps mitochondrial function, all the variety of different things within the cell, subcellular organelles and systems, and it’s only when you get a series of events, four or five or six, who knows? – where then the disease is triggered. But the important consequence of that is that it was triggered in one place; how can it propagate? How can it move away from that first area of seeding?
There are numerous possible explanations; the most fashionable is that this is a prion-like process. What people mean by that is that misfolded protein in one cell serves as the seed for misfolding, as a template for misfolding in other cells, and it, therefore, moves from cell to cell. Actually, I think there are all sorts of reasons why one should be cautious about concluding that’s what’s going on. Much of the evidence comes from rather in vitro forced experiments. In patients, what you see is constrained progression through the motor system, so they have particular, rather discreet and characteristic stereotyped patterns of evolution.
So ALS, therefore, is complex biologically even though clinically it looks like one thing, and Charcot and I could quite easily agree on the diagnosis. But what we now know is that there are numerous complex biological pathways that converge to create this disease, and that really tells you why it’s so difficult to treat. It’s difficult to treat because of the complexity; it’s difficult to treat because, by the time the patient comes to see you in the clinic with weakness in one area of the body, they almost certainly have exhausted their intrinsic reserve. The reserve capacity in the nervous system means you can lose function, and then when you present clinically, that is the point at which you’ve used up your intrinsic reserve. What you’re always seeing, even in the mildest cases, is the end stage of a process that may have been going on for a lot longer.

Professor of Neurology, Neurosurgery and Biomedical Engineering at McGill University Sylvain Baillet on brain ...

Meteorologist Chris Brierley on the tropical cyclogenesis, the distribution of tropical cyclones on the planet...

Geneticist Steve Jones on the nature-nurture controversy, genetics of obesity and how can you solve genetic pr...