Graphene
Nanotechnologist Andrea Ferrari on the properties of Graphene, its significant history, and how to send it fro...
Is cancer curable? What does it mean to cure cancer? These and other questions are answered by a Professor of Cancer Medicine and Oncology at the Imperial College London, Justin Stebbing.
Cancer means many different things to many different people, but the reality is that cancer is a disease of age, which means that it predominantly affects older people. We’re all living a lot longer because of general improvements in our standard of living, so now, one in two people gets cancer. As well as age, there are many other causes of cancer. People can have family histories and genes that can cause cancers or lead to cancers; heavy smoking and excessive alcohol consumption, obesity and even other diseases can lead to the development of cancers. Also, there are environmental hazards as well that are associated with cancer.
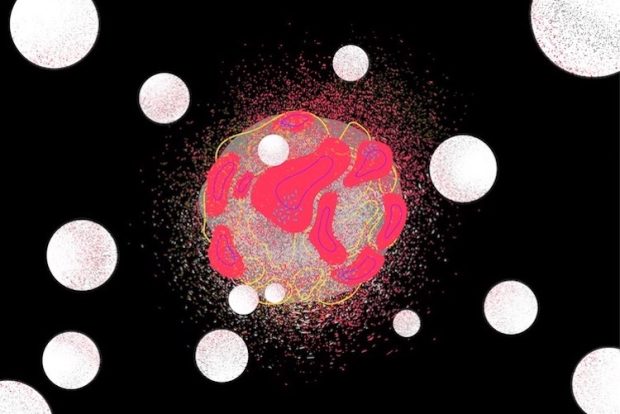
Cancers can be rapidly proliferative and very, very dangerous, and cancers can be very slow-growing as well. Often, detecting cancer earlier is associated with a better outcome, so we have screening programs for diseases such as breast cancer, colon cancer and cervical cancer where we try and detect it in its earlier stages. But cancer means different things to different people. People use terms such as ‘tumours’ or ‘neoplasia’, or ‘uncontrollable growths’. It used to have a stigma associated with it, so no one would talk about it, but now, as science advances, our health advances, and we have issues in society that have gone away, people, I think, are much freer to talk about cancer. We can often cure cancers, and some cancers are completely curable: the definition of cure means living to old age and dying of something else. Other cancers, particularly when cancers have spread, are not curable: in those cases, we try to keep the cancers under control so people live with them and don’t die from them. Sometimes, we use analogies such as diabetes or high blood pressure, where people live with these diseases and don’t die of these diseases.
In terms of treatment of cancer, there are many different types of treatment for cancer. Surgery is really important if it’s detected early enough. I specialize in the use of drugs to treat cancers: medicines such as immunotherapies which don’t stimulate the immune system; they inhibit the inhibition of the immune system because cancer can turn the immune system off. Other people use radiotherapy to treat cancers. We describe the combination, for example, of surgery, radiotherapy, chemotherapy, immunotherapy, hormonal therapy and all the different types of therapy and surgeries as a multidisciplinary approach where we have a team approach to treating cancer.
So even if we can’t cure it, the aim is that people live with it for many, many years.
The idea is to personalize treatment which means treating the right person with the right tumour at the right time with the right treatments.
It is difficult from one individual to the next: it depends on individual factors such as what people want for themselves, and it depends on tumour factors such as whether you can use those treatments not just to improve the quantity of life but to increase the quality of life as well because having one without another is not very useful.
Developments in oncology, though, are occurring at supersonic speed. One reason I became an oncologist was to combine research and patient care to link what we call the bench to the bedside. So, nowadays, we’re talking about personalization of treatment, which means treating the right person with the right tumour at the right time with the right treatment. I think of the use of medicines, surgery, and radiotherapy together to try and maximize the cure rate and, even if we can’t do that, to maximize survival with a good quality of life. However, it should be a team approach amongst different doctors and healthcare professionals along with treating a patient and their families.
We still sometimes need to use chemotherapy. I sometimes think of a cancer cell like the London Underground subway tube map, and I’m trying to work out if it is Charing Cross and Victoria that isn’t working or Waterloo, East Acton, Chalk Farm (Camden) and Embankment. And if we work out the subway stations that aren’t working, we can use targeted therapies to attack those subway systems or those individual subway stations. Cancer cells are clever, and they can find ways around that; they can find different loose, but it’s great that we can now use targeted therapies which are much more precise, have fewer side effects, and patients do much better on them. Examples include things like the ALK inhibitors in lung cancer or the anti-PD1 or anti-PDL1 immunotherapies. In patients for whom those are suitable, they really have transformed the lives of people with cancer. In the old days, people used to die really rapidly from things like metastatic lung cancer and other diseases such as that; nowadays, based on findings and the laboratory translated into people, we can really transform the lives of these people. So we now expect someone with metastatic melanoma, for example, to live more than five years with these remarkable drugs that aren’t just focused on killing cancer but are focused on strengthening our own immune systems as well. We like to take a holistic approach to treatment: it’s not just about the drugs and the surgery and the radiotherapy; it’s really important that patients are fit, they have the right diet, they have the right constitution, so the quality of life goes hand-in-hand with the quantity of life.
Some cancers, though, don’t cause many problems anyway; they can be very, very slow-growing. Cancer is a bit of a marketing term which is used to describe anything from pancreatic cancer that can spread very rapidly through us with survivals measurable in months to a little skin cancer that’s never going to cause a problem anyway. Going forward, it’s really important in conjunction with patients and their families to understand the type of cancer someone has so you can work out how best to treat it. And if you work out how best to treat it, we’re usually prolonging survival as much as possible with a good quality of life.
As an oncologist, every day, I’m learning about people and their families, and I’m learning about cancer.
If the road to really cure cancer is one mile long, we’re probably 10 feet into it.
I really don’t understand how and why cancer spreads or why it happens in a disease as simple as breast cancer. For example, a woman may have two breaths usually, the same family history, and the same genes, but only one bit of one breast gets cancer, for example. Why does that occur? Why does it spread to the locations it spreads? Why does it spread in the pattern of spread that we see? And really, why our treatment doesn’t eradicate all cancer cells? Why can cancers recur many, many years later? We know that cancer stem cells can exist, a bit like a queen bee it can repopulate a nest 8-10 years later, but what we really need to know and what we really need to understand is why cancers happen to some people and how best to treat them to eradicate them? It’s still the reality that once a cancer such as breast, colon, prostate or lung cancer, the common cancers, have spread, we no longer consider them curable. What makes them incurable, why they are incurable, and what we can do to increase the cure rate are questions that I ask every single day.

Nanotechnologist Andrea Ferrari on the properties of Graphene, its significant history, and how to send it fro...

Bioengineer Ali Khademhosseini on cells' environment, gene circuits, and directing differentiation

Oncologist Justin Stebbing on different types of treatment for cancer, gene sequencing and what does it mean t...