Brain Training
Neuropsychologist Barbara Sahakian on cognitive training, areas of the brain that get affected in Alzheimer's ...
Huntington’s disease is a devastating autosomal dominant neurodegenerative disorder. In this type of genetic condition, the chance of an affected individual passing on the disease to any one of their children is 50%. Besides Huntington’s disease is one of the most common neurological diseases caused by a single gene mutation, there are features of this disease that are shared by a number of other neurodegenerative diseases, like Alzheimer’s disease and Parkinson’s disease. In all of these diseases, one sees the deposition of proteins in aggregates in the nerve cells.
Huntington’s disease is caused by a CAG trinucleotide repeat expansion in the gene encoding the protein huntingtin. Unaffected individuals have a stretch of CAG repeats in their genes that has fewer than 36 repeats – so this would look like CAGCAGCAGCAGCAGCAGCAGCAGCAGCAG…People with Huntington’s disease have 36 or more of these repeats. As CAG in these repeats is translated into the amino acid glutamine, the mutant huntingtin protein has an abnormally long polyglutamine tract. This type of mutation is seen in 8 other neurodegenerative diseases.

The expanded polyglutamine tract confers toxic properties onto huntingtin. These may affect many different systems and may be related to the propensity of the mutant protein to aggregate or sequester many other proteins from their normal functions in the cell. This results in neurodegeneration, most prominently in the caudate, putamen, and cerebral cortex.
At a clinical level, patients develop abnormal movements, cognitive deterioration (a form of dementia), and psychiatric manifestations. The most obvious movement disorder seen in Huntington’s is called chorea, which describes abnormal involuntary movements that are brief and irregular. Importantly, the psychiatric symptoms of this disease, like depression, are part of the disease’s biology and not always simply a response to having the disease. The disease typically presents in middle age with a median onset of around 40 years. However, in cases with a very long repeat expansion, the disease can present in early childhood, while in some cases with repeat expansions closer to the 36 CAG repeat cutoff may present late in life – disease onset tends to be earlier with longer trinucleotide repeat expansions. While there can be some variation in the disease presentation with regards to which features may be most prominent early in the disease, the disease signs are fairly well encapsulated by the typical signs that patients show. The disease course is about 15-20 years until death.

The disease is named after the American physician George Huntington, who described the condition in detail in 1872. In the first of the two papers he authored, entitled “On Chorea”, he carefully described the features of the disease from observations he had made in a family with this condition who lived in Long Island. However, earlier descriptions exist. The initial linkage of the disease gene to the short arm of human chromosome 4 by James Gusella and colleagues provided an early classical example of how one can locate the site of a gene on a specific chromosomal location by studying families. The subsequent identification of the mutation and the disease gene by Gusella and a large consortium enabled subsequent precise genetic testing and provided the key resource for modeling the disease in cells and animals, which is crucial for therapeutic development.
At present, there are no treatments that are known to modify neurodegeneration in humans. However, tetrabenazine can reduce some of the movement abnormalities in the disease. Tetrabenazine is not believed to reduce the rate of neurodegeneration in Huntington’s disease. Chorea is caused by an excess of the neurotransmitter dopamine, and tetrabenazine reduces this symptom by lowering the activity of dopamine in the brain.
Numerous methods are being pursued to treat Huntington’s disease at a mechanistic level, including strategies to decrease the expression of the mutant protein with antisense methods (in clinical trials) and autophagy upregulation. Antisense strategies involve oligonucleotide nucleic acids that have sequences that are complementary to the Huntington’s disease gene and which reduce the amount of huntingtin that is synthesized. This is a rational strategy as the prime driver for the disease is mutant huntingtin.
The disease affects about 1/10,000 people in populations of European descent. However, it is more common in some population isolates (in Venezuela) and is rarer in some populations (e.g., Japanese). The variation in prevalence in different populations is a consequence of the number of gene carriers in these groups. This is a consequence of historical events, including chance increases/decreases of Huntington’s disease carriers in population isolates.

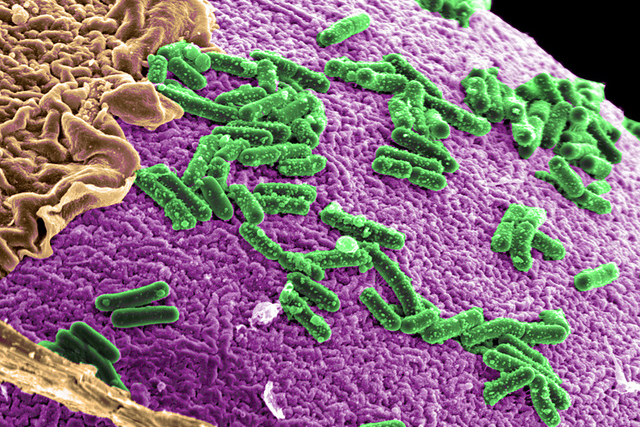
My laboratory has focused on the protective roles of autophagy in Huntington’s disease and related neurodegenerative conditions. Autophagy is a process that cells use in order to degrade parts of the cytoplasm by engulfing them in vesicles, called autophagosomes, which are then transported to the lysosomes. After the autophagosomes fuse with lysosomes, the enzymes in the lysosomes degrade the autophagic contents. We discovered that those intracellular aggregate-prone proteins, like mutant huntingtin, are autophagy substrates. Importantly, we were the first to show that drugs that increase autophagy enhance the removal of toxic proteins like mutant huntingtin, mutant ataxin 3 (that causes the most common spinocerebellar ataxia), alpha-synuclein (in Parkinson’s disease) and mutant and wild-type forms of tau (relevant to Alzheimer’s disease and forms of frontotemporal dementia).
We have extended our studies from cell-based systems to showing the efficacies of such drugs in the fruit fly, zebrafish, and mouse models of such diseases. This concept has been subsequently validated in diverse neurodegenerative diseases by many groups. Our vision is to develop this strategy into a clinical reality, and we have undertaken a number of studies to identify new pathways and drugs that can induce autophagy. Indeed, with my colleague Dr. Roger Barker, we recently completed a safety trial with one of the drugs we identified in Huntington’s disease patients.
There are many current research projects that are ongoing and contributing to the study of the disease. There is significant activity in the following areas: First, how does mutant huntingtin cause disease? This is being approached via different methods, including structural biology, biophysics, genetic screens, cell biology, and animal modeling. Some groups are focusing on the disease at a biochemical level by trying to discern the structure of the mutant protein and its early aggregating species. Others are using cell, neuronal, and stem cell models to understand the pathways that are perturbed by the mutant protein. These are complemented by animal studies in worms, fruit flies, zebrafish, mice, rats, and even primates and sheep, to develop models to understand disease at an organismal level and to have models to test therapeutic strategies.
Secondly, what are the functions of normal huntingtin? These functions are still poorly understood. Groups are using a range of cell model-based approaches to elucidate these functions. These may influence therapeutic strategies and/or influence our general understanding of how cells work.
Third, the identification of novel potential therapeutic targets to ameliorate disease and refinement of existing strategies with promise. Various groups are attacking this problem using chemical and genetic screening approaches to identify novel targets and potential drugs.
Fourth, identification and characterization of biomarkers of disease progression to facilitate clinical trials. In order to be able to track the possible benefits of any therapeutic strategy, it is powerful to have measures of disease progression that are highly sensitive and that change in short periods of time. This is particularly important for individuals who have the disease gene but do not have overt signs and symptoms, as one may be able to test the effects of potential therapeutics that can delay the onset of the disease.
Edited by John Mark Shorack

Neuropsychologist Barbara Sahakian on cognitive training, areas of the brain that get affected in Alzheimer's ...
Prof. Jeff Lichtman of Harvard University on the neuromuscular junction, loss of axon connections, and 'brainb...

New research sheds light on the evolution of complex animal groups, suggesting that they may have evolved earl...