Genome Medicine
Bioinformatician Tim Hubbard on the ‘100,000 Genomes Project’, how to use genome data in diagnostics and treat...

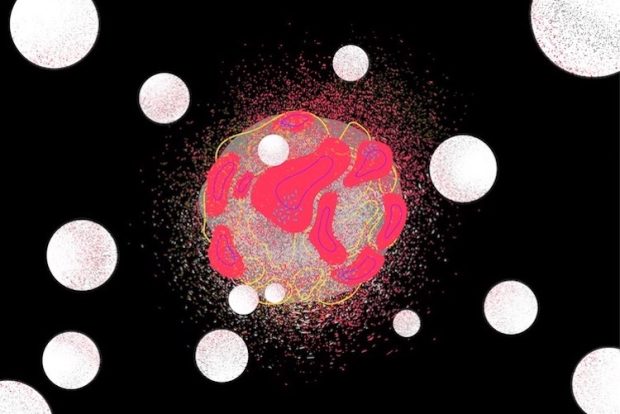
Photodynamic therapy is a phenomenon that has been known for a very long time. If you excite a molecule photochemically, you produce its excited state, which can pass on its energy to oxygen and produce a special form of oxygen, singlet oxygen, which is very reactive with anything around it. If that happens to be in a human cell, it will destroy that cell. This characteristic is called phototoxicity. As the subject has developed, photodynamic therapy has been used to destroy cancer cells and treat cancer.
The technique is very simple: you inject a dyestuff into the bloodstream, which travels around the body and is designed to locate preferentially in cancer cells of tumor tissue. Then you turn on a red laser, which excites the molecule, and you get this process, where singlet oxygen is produced. It will destroy that cell and the whole tissue around it. In this way, it is used to treat cancer.
You need certain requirements in the sensitizer that you use – it has to absorb red light. You can demonstrate this for yourself: if you put your hand over a torch, you know that only red light is transmitted through your flesh (your fingers will look red). So, if you want to get light into human tissue, you have to use red light because that is the only color that is not absorbed by other tissue. You need a dye that absorbs red light; it has to be effective in producing oxygen, which will kill the tissue. It should have some preference for tumor tissue compared with normal tissue; it should be lost relatively easily from the body because if it stays in the body for too long, it will get into the skin, and if you then go out in sunlight, you will get damage, which you don’t want. These are the four main requirements. Of course, it should not be toxic on its own. It should only be toxic when you excite it with the light.
There are many molecules that answer these criteria and which are useful. The first that was developed was a component called hematoporphyrin derivative, porphyrins of flat plate-like molecules. The molecules we worked on in competition with a Russian group from the Institute for Chemical Physics are phthalocyanine, which is related really much to porphyrins.
These molecules can form stacks. Unfortunately, those stacks of molecules are not photochemically active, whereas we want them to be so. One of the ways to prevent staking is to put a solubilizing group, that is, to change the structure chemically. Therefore, you make the molecule easily dissolve in water. It is easy to deliver in the body, but also it stops stacking, which means you can build up a concentration of material, which will be useful when you turn the laser on.
We use molecules called phthalocyanine, which are just dyestuffs essentially. In the middle of this plate, they have an aluminum atom. That helps to prevent stacking as well. We used a sulfonate group, which is just sulfur and three oxygens. At the same time, the group in Moscow was looking at exactly the same process. We decided that the best molecule for our use was disulfonate, a molecule that has two sulfonate groups. It becomes amphiphilic: one end of the molecule dissolves in water, and the other end of the molecule dissolves in fat, so it is slotted into cell membranes. A Russian group used tri-sulfonated and tetra-sulfonated materials, which were much more water-soluble than ours. Both are in use.
What happens in either case? You inject the dye into the bloodstream; a dye locates in the tumor, and you turn on the red laser, which will then turn on the chemistry, which destroys the tumor. So, you have to be able to get the light where you want it. The easiest place to get to is the skin. That is why skin cancers can be treated very readily with this. You can deliver light through a fiber (a colonoscope or a gastroscope, or equivalence), so you can get into any hollow organ in the body. A gastroscope goes down through your mouth into your stomach; a colonoscope goes up the other end. These techniques have been very successful, too – tens of thousands of patients worldwide have been treated using this photodynamic therapy.
There are limits to which tumors you can use and which you can destroy. In brain tumors, you have to open the skull, so you can treat a surface brain tumor, but not the one which is deep in the brain. In the case of pancreatic tumors, which are really deadly, you have to insert fibers into the pancreas (approximately eight fibers through a needle), but then it works and destroys the tumor.
The one organ you cannot treat is the liver because the normal process by which the dye is lost from the body is excreted through the liver. If you inject somebody with the dye, the normal leaver will contain a very large amount of it. If you turn on the laser, you will destroy the liver with catastrophic consequences. For this reason, you may not use it for liver cancer. You also cannot apply it systemically – you cannot treat the whole body; you have to put the laser light where you want in the tumor.
Many dyestuffs are available and are used throughout the world, including aluminum phthalocyanine. We thought that photochemically we had got to a good enough state; there were enough sensitizing molecules available, and things were not going to improve by marginal improvements in singlet oxygen.
What else could you do to make this whole process much more efficient? You could target the dye onto tumor cells preferentially. There are various ways of doing that. You can use a monoclonal antibody (or a fragment of a monoclonal antibody), some proteins, molecules of folic acid, or nanostructured materials. We chose the monoclonal antibody fragment, and we have been able to deliver as many as 10-12 molecules of dye staff preferentially to a cell because we choose targets that are in access in tumor tissue compared with normal tissue. Monoclonal antibody fragment targets that type of cell, taking with it the dyestuff. When you turn on the laser, and you only destroy the tumor tissue, not the normal tissue.
With the targeted approach using monoclonal antibody fragments, we can get a contrast ratio of 60 or 100 to 1. So, there is no damage to normal tissue at all. The other advantage is that monoclonal antibody with dyestuff added is lost fairly quickly from the body. Within 24 hours of injection, the body is clear of this dyestuff. You do not have any restrictions beyond 24 hours of going out in sunlight. With some of the earlier sensitizers, you actually had to stay indoors for many months just to be on the safe side. These are huge advantages of that.

Bioinformatician Tim Hubbard on the ‘100,000 Genomes Project’, how to use genome data in diagnostics and treat...

Richard Henderson on the advantages of cryomicroscopy, factors limiting new discoveries, and the history of mo...

Molecular Neurogeneticist David Rubinsztein on neurodegenerative diseases, stem cells, and fluorescent protein...