What Science Knows About Immunity: Innate, Adaptive, and More
Truth and myths about the structure and functioning of immunity
faq | July 3, 2024

Immunity is a complex, multicomponent system; only some fully understand how it works. A lack of knowledge about immunity principles often leads to magical thinking: We strive to “boost” our immunity and use terms like “weak immunity,” which, in reality, can be meaningless and even dangerous. What is immunity, and how does it work?
The Basics
Immunity is an ancient evolutionary system that emerged in living nature before dividing plants and animals into kingdoms. Plants and animals have their own immune systems. Immunity’s primary function is to protect against external invasions, such as viruses, bacteria, fungi, and more.
Immunity is divided into innate and adaptive (or acquired) immunity based on a simple criterion. Innate immunity does not require the immune system to learn; it reacts immediately upon recognizing something foreign. Innate immunity has a receptor apparatus from the host’s embryonic development. However, innate immunity has little to no memory function, so it responds to any new invasion like before. Thus, innate immunity is not very diverse and is often nonspecific.
Evolutionarily, the emergence of innate immunity is linked to nutrition: the feeding of unicellular organisms involves phagocytosis, a process that is a fundamental element of innate immunity.
As multicellularity and the evolution of pathogens developed, there was a need for more sophisticated regulatory mechanisms, leading to the formation of adaptive immunity, aptly named because it adapts to the invasion of a parasite. The first encounter results in a slow and weak response, but upon repeated contact, the immune system is trained, its receptors are tuned to a specific type of invasion, and the organism fights more robustly and efficiently. This requires a receptor apparatus that is much more complex than in the first case.
Science does not know precisely when adaptive immunity evolved. However, adaptive immune systems are already present in bony fish — indicating that the emergence of adaptive immunity likely occurred during the formation of the fish class.
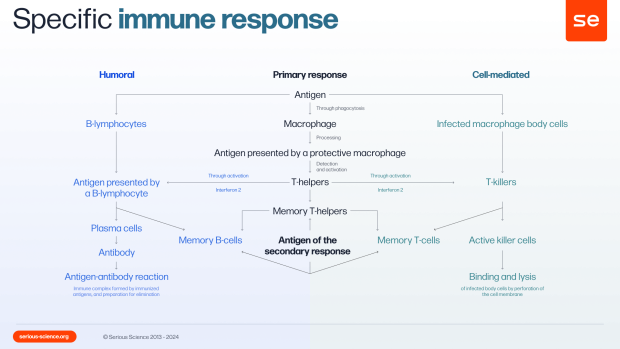
Another classification divides immunity into cellular and humoral immunity. Cellular immunity involves immune responses carried out by the immune system’s agent cells: they destroy foreign bodies on the surface and inside the cells. Examples include lymphocytes (B-cells, T-cells) and phagocytes (macrophages, monocytes, dendritic cells).
Humoral immunity involves agents secreted by cells entering the intercellular space to search for and combat pathogens. Antibodies play a crucial role in the humoral immune response.
Antibodies are large proteins in blood plasma produced by the adaptive immune system after encountering a specific pathogen. Once formed, antibodies remain in the body for a long time, helping to prevent future infections. However, antibodies are not only naturally occurring. Today, they can also be synthesized in the laboratory — these are known as monoclonal antibodies, which are used particularly when the body’s own antibody response is insufficient. These antibodies are highly specific, working against particular strains of a given pathogen. Therefore, with new circulating variants, these drugs must be updated and reintroduced into the body, ensuring their targeted action.
Organs of the Immune System
The most important organ of the immune system in humans is the bone marrow; this soft tissue is located in the spongy substance of bones and bone marrow cavities. In the bone marrow, crucial processes for the body occur — hematopoiesis and immunopoiesis — the maturation of all types of immune system cells. Some cells reach a ready-to-function state here: for example, neutrophils, which enter the bloodstream from the bone marrow, or monocytes, which also enter the bloodstream and can transform into macrophages in the organs. In the bone marrow, lymphocytes are formed and then migrate to other areas of the body, where they undergo selection for subsequent functioning as immune system cells.
For example, T-lymphocytes move to another central organ of the immune system — the thymus, a gland located behind the sternum. All lymphocytes that strongly react to “self” are destroyed, and T-cells that poorly recognize foreign elements are selected. As a result, 95% of the cells perish here, while the remaining 5% move to the periphery — to the lymphatic system, settle in the spleen and lymph nodes, and are ready to receive signals from cells that first contact the pathogen.
The Connection Between Innate and Adaptive Immunity
When we say that adaptive immunity begins to work when innate immunity needs it, the question arises about the signalling connection between the two systems. Scientific research only shed light on the interaction mechanism in the 1990s and 2000s.
However, relatively recent studies were only possible with the fundamental work of past centuries. The first significant work in this direction was by the biologist Ilya Mechnikov, who discovered phagocytosis in 1882 — a process by which cells (protozoa or specially designated blood and tissue cells — phagocytes) capture and digest solid particles. During this period, immunologist Paul Ehrlich played a fundamental role by discovering specific protective proteins produced by immune lymphocytes, which he named antibodies.
Later, American immunologist Charles Janeway and his students formulated several principles on how phagocytes (agents of innate immunity) interact with elements of adaptive immunity — primarily T- and B-lymphocytes.
During this period, the crucial role of dendritic cells — one type of phagocyte — was understood. Dendritic cells can phagocytize, process the phagocytized material, and continuously, without external stimuli, present antigens of ingested bacteria or viruses to lymphatic system cells — T-cells. Suppose all phagocytes are considered innate immune cells, and T-lymphocytes are part of the adaptive immune system. In that case, it turns out that dendritic cells are the main link between innate and adaptive immunity.
New molecules participating in the interaction of the two systems are discovered every year, but the fundamental concepts of their connection were established at the turn of the century.
“Strengthening” the Immune System
As we can see, immunity is multi-component and complex; therefore, influencing this system with a specific focus is advisable. For example, a specific immunodeficiency can be identified: a deficiency in antibody production to a specific pathogen, for instance — and targeted actions can be taken to increase their concentration. The insufficient functionality of T-cells can be detected, and appropriate methods can be developed for that case. The general concept of strengthening immunity is immunologically meaningless, and unconsidered interference in this system can be dangerous to health and life.
There are well-known practical examples: after the discovery of corticosteroids, these hormones were widely used for tuberculosis to reduce lung inflammation. They effectively suppress inflammation mediators, but systemic administration of corticosteroids in sufficient doses to solve the problem also suppresses a broad class of biochemical reactions necessary for the body’s existence. This practice was later abandoned worldwide, and now corticosteroids are applied only locally and in limited amounts, for example, in bronchial asthma.
If a patient seeks general care for their immune system, recommendations that generally positively affect health may be applicable. These include a varied diet with vegetables, fruits, meat, and fish, moderate physical activity, and a proper sleep and wake schedule.
In normal functioning, the immune system is accompanied by the constant support of molecular mechanisms that remove cell clones capable of responding to self-antigens from the body. However, as with any complex system, there can be numerous failures. In some cases, these failures lead to autoimmunity or an excessive immune response — a situation where the immune system begins recognising and responding to its tissues. This process can result in diseases such as systemic lupus erythematosus, rheumatoid arthritis, and autoimmune diabetes. These conditions have a variety of genetic causes. On the other hand, there is the opposite process known as immunodeficiency. This disorder of immunological reactivity occurs due to the loss of one or more components of the immune apparatus, leading to a weakened immune system.
The Matter of Evolution
The evolution of the immune system is a significant process that has shaped the survival and adaptation of different classes of animals. For instance, the more advanced immune response system of mammals compared to amphibians and the similar effectiveness of immune responses in rodents and primates highlight the importance of this evolutionary journey. This evolution has led to warm-blooded animals possessing a more complex and advanced immune apparatus than their ancestors — fish or amphibians.
Therefore, the human immune apparatus is the product of a long evolutionary process. As a result, a mechanism was formed, divided into innate and acquired immunity, and scientists have obtained a relatively recent understanding of the connection between these two types of immune response. The effectiveness of various immune response components can be explicitly evaluated and quantitatively: for this reason, general terms such as “strong” or “weak” immunity are meaningless. It is more appropriate to use a specific term — immunodeficiency — a disorder caused by losing one or more components of the immune apparatus.
This article is developed in collaboration with the biopharmaceutical company AstraZeneca.